Russian Fluoridation Research
Laxmidhar Panda, Dr. B.B. Kar & Dr. B. B. Patra
Research Scholars, School of Applied Sciences,
KIIT University, Bhbaneswar, Odisha, India
Key words: Fluorosis, Fluoroapatite,
Biomineralisation, Calcification, Osteosclerosis.
…Excess fluoride may lead to an increased demineralization
leading to the precipitation of Calcium phosphate and
Calcium fluoride and it interferes with calcium metabolism…
→ The Ten Major Fluorides ←
TGA Updates – July 2019 + Interpretation
Osaka Japan – Sars – & Covid-19 – cure – [new research]
Black Tea Source, Production, & Consumption:
Assessment of Health Risks of Fluoride Intake In New Zealand +
50 Tons of Cures for Coronavirus – China – Vitamin C
… Higher levels of aluminium and fluoride
were related to dementia risk in a population of men and
women who consumed relatively low drinking-water levels of both …
Aluminium & Fluoride in Drinking Water in Relation to Later Dementia Risk
Ameliorative Effects of Quercetin on Sodium Fluoride-Induced
Oxidative Stress in Rat’s Kidney
Avid Science – Richard Sauerheber
Fluorosis, unsightly at best, was found to afflict
5 million U.S. teenagers aged 12-15 as of 2004
FLUORIDE AND OXIDATIVE STRESS
This thesis draws together research outcomes for sites
predominantly throughout Queensland, Australia.
A great work – We thank you !
This paper does not mention fluoride but it needs to be considered
with previous research into Underground Water in Queensland.
Fluorides and radioactive materials
are a deadly combination.
Full original text → HERE
See also↓
→ Atomic Tests in Australia ←
↑ If you ever needed evidence that people ↑
in high places lie, here it is.

Fluoride Causes Heart Disease, Stroke and Sudden Death
Full text → HERE
This brief survey shows that hundreds of scientists have studied the toxic impact of Fluoride on the
cardiovascular system for over 70 years and the detailed evidence of harm is overwhelming.
The general public needs to be warned to minimize their total Fluoride intake. Especially
vulnerable groups such as the unborn, diabetics and those with compromised
kidneys or thyroid must be protected. Promotion of Fluoride and
Fluoridation must cease.
Politicians must purge the bureaucracy of Fluoride promoters.
Not a single excess death caused by water fluoridation can be tolerated.
FISH !
… Millions of salmon have instinctively know this for thousands
of years, that is why they go to so much trouble
to swim up rivers to lay their eggs
in fluoride free water.
(Sea water contains fluoride.)
Professor Paul Engelking says fish and fluoride don’t mix.
THIS IS A GREAT VIDEO ⇒ HERE ⇐ A slow start but stay with it!
Zürich Statement on Future Actions on Per-
and Polyfluoroalkyl Substances (PFASs)
FISH LICE COULD BE EARLY INDICATORS OF
METAL POLLUTION IN FRESHWATER
Since 2006, epidemiological studies have documented
six additional developmental neurotoxicants—manganese,
fluoride, chlorpyrifos, dichlorodiphenyltrichloroethane,
tetrachloroethylene, and the polybrominated diphenyl ethers.
“FLUORIDE POLLUTION AND ITS EFFECT ON WATER AND
VEGETATION IN BIRBHUM DISTRICT, WEST BENGAL”
Mind-blowing interview with Judy Mikovits, PhD
Taken down!
TRY → HERE
In 2014, She co-authored,
“Plague: One Scientist’s Intrepid Search for the
Truth about Human Retroviruses & Chronic Fatigue Syndrome”
9 More Vaccine Ingredients
Water Fluoridation: Risky Business for Council-Michael Lusk
Dr. Richard Sauerheber-Formally apologises to the European Union
Lawsuit Reveals How Paid Expert Helped 3M
“Command the Science” on Dangerous Chemicals
FACTORS OFTEN OVERLOOKED IN FLUORIDATION RESEARCH
XXXIst CONFERENCE ADVANCES IN FLUORIDE RESEARCH
Very Old Research – 80+ years ↓
Rat Research – Fluoride 1934 – U.S. Dept. of Agriculture
Work in this laboratory has shown that fluorine interferes
with the normal development of teeth and bones…
$hame On $low $cience
Lawsuit Reveals How Paid Expert Helped 3M “Command the Science”
The Third Digital Revolution to Unleash the Power of Anti-Censorship
THE HISTORY OF WESTERN MEDICAL/VACCINE INDUSTRIES
Perchlorate Abundant In Desert –
The Relationship between fluoride concentration in drinking
water and mortality rate from uterine cancer
in Okinawa prefecture, Japan
Prenatal Fluoride Exposure and Cognitive Outcomes in
Children at 4 and 6–12 Years of Age in Mexico
Fluoride Is The Major CauseOf Cataract Blindness
How Understanding Epigenetics Can Save Your Life
New perspective on metals and other contaminants in fluoridation chemicals
Effectiveness Of Fluoride Varnish…
→ BIASES – EXAMPLES IN THE 2016 NHMRC DRAFT REPORT ←
See also:
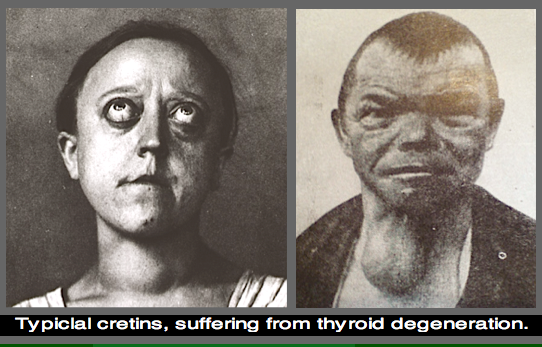
— FLUOROSIS —
COAL BURNING – CHINA
106 Fluoride Vol. 36 No. 2 106-112 2003 Research Report
My Views on the Fluoridation of Water
Fluoridation, 1979 Scientific Criticisms and Dangers
by
Philip R.N. Sutton Former Senior Lecturer in Dental Science
University of Melbourne Australia
→ Fluoridation Philip Sutton ←
An Inconvenient Tooth – Fluoride Documentary
↓ ↓ ↓
http://www.youtube.com/watch?v=sh-oeu2L8yM&feature=player_embedded
FLUORIDE IN DRINKING WATER:
A Scientific Review of EPA’s Standards
by
Committee on Fluoride in Drinking Water
Board on Environmental Studies and Toxicology
Division on Earth and Life Studies
NATIONAL RESEARCH COUNCIL OF THE NATIONAL ACADEMIES
→ → NRC_2006 ← ←
SEE OUR COMPILATION ON LEAD AND FLUORIDES → HERE
See also → ATRAZINE AND CHLORINE.
Plumb-solvency Exacerbated by Fluoridation-Dr. Geoff Pain
WATER -Stroke & Heart Attacks – a short read
Fluorosis in 89% Carnarvon Aborigines +
Bone/joint problems-Fluorosis
You may not be able to imagine that borax, this humble insecticide
and laundry detergent, has the potential of singlehandedly
bringing down our entire economic system ! ↓
THE BORAX CONSPIRACY
~ DISCLAIMER ~
Some of the articles or pieces posted on this site contain copyrighted material.
Credit is given to the author and links are provided to the original source.
We believe that this constitutes a ‘fair use’.
The peoples of the world have a right to true science.
Deceit and fake $cience need to be exposed.
… Untested chemicals should not be presumed to be safe
to brain development, and chemicals in existing use
and all new chemicals must therefore be tested
for developmental neurotoxicity …
ORIGINAL → HERE ←
Review
Lancet Neurol 2014; 13: 330–38
Published Online
February 15, 2014
http://dx.doi.org/10.1016/
S1474-4422(13)70278-3
Department of Environmental Medicine,
University of Southern Denmark,
Odense, Denmark (P Grandjean MD);
Department of Environmental Health,
Harvard School of Public Health, Boston, MA, USA
(P Grandjean); and Icahn School of Medicine at Mount Sinai,
New York, NY, USA
(P J Landrigan MD)
Correspondence to:
Dr Philippe Grandjean,
Environmental and Occupational Medicine and Epidemiology,
Harvard School of Public Health,
401 Park Drive E-110, Boston,
MA 02215, USA
pgrand@hsph.harvard.edu
Neurobehavioural effects of developmental toxicity
Philippe Grandjean, Philip J Landrigan
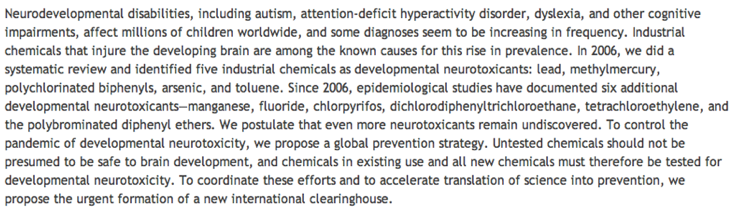
Neurodevelopmental disabilities, including autism, attention-deficit hyperactivity disorder, dyslexia, and other cognitive impairments, affect millions of children worldwide, and some diagnoses seem to be increasing in frequency.
Industrial chemicals that injure the developing brain are among the known causes for this rise in prevalence.
In 2006, we did a systematic review and identified five industrial chemicals as developmental neurotoxicants:
lead, methylmercury, polychlorinated biphenyls, arsenic, and toluene.
Since 2006, epidemiological studies have documented six additional developmental neurotoxicants—manganese, fluoride, chlorpyrifos, dichlorodiphenyltrichloroethane, tetrachloroethylene, and the polybrominated diphenyl ethers.
We postulate that even more neurotoxicants remain undiscovered.
To control the pandemic of developmental neurotoxicity, we propose a global prevention strategy.
Untested chemicals should not be presumed to be safe to brain development, and chemicals in existing use and all new chemicals must therefore be tested for developmental neurotoxicity. To coordinate these efforts and to accelerate translation of science into prevention, we propose the urgent formation of a new international clearinghouse.
Introduction
Disorders of neurobehavioural development aff ect 10–15% of all births,1 and prevalence rates of autism spectrum
disorder and attention-deficit hyperactivity disorder seem to be increasing worldwide.2 Subclinical decrements in
brain function are even more common than these neurobehavioural developmental disorders.
All these disabilities can have severe consequences3—they diminish quality of life, reduce academic achievement, and disturb
behaviour, with profound consequences for the welfare and productivity of entire societies.4
The root causes of the present global pandemic of neurodevelopmental disorders are only partly
understood. Although genetic factors have a role,5 they cannot explain recent increases in reported prevalence,
and none of the genes discovered so far seem to be responsible for more than a small proportion of cases.5
Overall, genetic factors seem to account for no more than perhaps 30–40% of all cases of neurodevelopment disorders. Thus, non-genetic, environmental exposures are involved in causation, in some cases probably by interacting with genetically inherited predispositions.
Strong evidence exists that industrial chemicals widely disseminated in the environment are important contributors to what we have called the global, silent pandemic of neurodevelopmental toxicity.6,7
The developing human brain is uniquely vulnerable to toxic chemical exposures, and major windows of
developmental vulnerability occur in utero and during infancy and early childhood.8 During these sensitive life stages, chemicals can cause permanent brain injury at low levels of exposure that would have little or no adverse effect in an adult.
In 2006, we did a systematic review of the published clinical and epidemiological studies into the neurotoxicity of industrial chemicals, with a focus on developmental neurotoxicity.6
We identified five industrial chemicals that could be reliably classified as developmental neurotoxicants: lead, methylmercury, arsenic, polychlorinated biphenyls, and toluene.
We also noted 201 chemicals that had been reported to cause injury to the nervous system in adults, mostly in connection with occupational exposures, poisoning incidents, or suicide attempts. Additionally, more than 1000 chemicals have been reported to be neurotoxic in animals in laboratory studies.
We noted that recognition of the risks of industrial chemicals to brain development has historically needed decades of research and scrutiny, as shown in the cases of lead and methylmercury.9,10
In most cases, discovery began with clinical diagnosis of poisoning in workers and episodes of high-dose exposure. More sophisticated epidemiological studies typically began only much later.
Results from such studies documented developmental neurotoxicity at much lower exposure levels than had previously been thought to be safe. Thus, recognition of widespread subclinical toxicity often did not occur until decades after the initial evidence of neurotoxicity.
A recurring theme was that early warnings of subclinical neurotoxicity were often ignored or even dismissed.11
David P Rall, former Director of the US National Institute of Environmental Health Sciences, once noted that “if thalidomide had caused a ten-point loss of intelligence quotient (IQ) instead of obvious birth defects of the limbs, it would probably still be on the market”.12 Many industrial chemicals marketed at present probably cause IQ deficits of far fewer than ten points and have therefore eluded detection so far, but their combined effects could have enormous consequences. In our 2006 review, 6 we expressed concern that additional developmental neurotoxicants might lurk undiscovered among the 201 chemicals then known to be neurotoxic to adult human beings and among the many thousands of pesticides, solvents, and other industrial chemicals in widespread use that had never been tested for neurodevelopmental toxicity. Since our previous review, new data have emerged about the vulnerability of the developing brain and the neurotoxicity of industrial chemicals. Particularly important new evidence derives from prospective epidemiological birth cohort studies.
In this Review, we consider recent information about the developmental neurotoxicity of industrial chemicals
page 330
www.thelancet.com/neurology Vol 13 March 2014
Review to update our previous report. 6 Additionally, we propose strategies to counter this pandemic and to prevent the spread of neurological disease and disability in children worldwide.
Unique vulnerability of the developing brain
The fetus is not well protected against industrial chemicals. The placenta does not block the passage of many environmental toxicants from the maternal to the fetal circulation,13 and more than 200 foreign chemicals have been detected in umbilical cord blood.14 Additionally, many environmental chemicals are transferred to the infant through human breastmilk.13 During fetal life and early infancy, the blood–brain barrier provides only partial protection against the entry of chemicals into the CNS.15
Moreover, the developing human brain is exceptionally sensitive to injury caused by toxic chemicals,6 and several developmental processes have been shown to be highly vulnerable to chemical toxicity. For example, in-vitro studies suggest that neural stem cells are very sensitive to neurotoxic substances such as methylmercury.16 Some pesticides inhibit cholinesterase function in the developing brain,17 thereby affecting the crucial regulatory role of acetylcholine before synapse formation.18 Early-life epigenetic changes are also known to affect subsequent gene expression in the brain.19 In summary, industrial chemicals known or suspected to be neurotoxic to adults are also likely to present risks to the developing brain.
Figure 1 shows the unique vulnerability of the brain during early life and indicates how developmental exposures to toxic chemicals are particularly likely to lead to functional deficits and disease later in life.
New findings about known hazards
Recent research on well-documented neurotoxicants has generated important new insights into the neurodevelopment consequences of early exposures to these industrial chemicals.
Joint analyses that gathered data for lead-associated IQ deficits from seven international studies20,21 support the conclusion that no safe level of exposure to lead exists.22
Cognitive deficits in adults who had previously shown lead-associated developmental delays at school age suggest that the effects of lead neurotoxicity are probably permanent.23 Brain imaging of young adults who had raised lead concentrations in their blood during childhood showed exposure-related decreases in brain volume.24 Lead exposure in early childhood is associated with reduced school performance25 and with delinquent behaviour later in life.26,27
Developmental neurotoxicity due to methyl-mercury occurs at much lower exposures than the concentrations that affect adult brain function.28 Deficits at 7 years of age that were linked to low-level prenatal exposures to methyl-mercury were still detectable at the age of 14 years.29 Some common genetic polymorphisms seem to increase the vulnerability of the developing brain to methyl-mercury toxicity.30 Functional MRI scans of people exposed prenatally to excess amounts of methyl-mercury showed abnormally expanded activation of brain regions in response to sensory stimulation and motor tasks (fi gure 2).31 Because some adverse effects might be counterbalanced by essential fatty acids from seafood, statistical adjustment for maternal diet during pregnancy results in stronger methylmercury eff ects.32,33
Prenatal and early postnatal exposures to inorganic arsenic from drinking water are associated with cognitive deficits that are apparent at school age.34,35 Infants who survived the Morinaga milk arsenic poisoning incident had highly raised risks of neurological disease during adult life.36
The developmental neurotoxicity of polychlorinated biphenyls has been consolidated and strengthened by recent fi ndings.37 Although little new information has been published about the developmental neurotoxicity of toluene, much has been learned about the developmental neurotoxicity of another common solvent, ethanol, through research on fetal alcohol exposure. Maternal consumption of alcohol during pregnancy, even in very small quantities, has been linked to a range of neurobehavioural adverse effects in off spring, including reduced IQ, impaired executive function and social judgment, delinquent behaviour, seizures, other neurological signs, and sensory problems.38
Newly recognised developmental neurotoxicants
Prospective epidemiological birth cohort studies make it possible to measure maternal or fetal exposures in real time during pregnancy as these exposures actually occur, thus generating unbiased information about the degree and timing of prenatal exposures. Children in these prospective studies are followed longitudinally and assessed with age-appropriate tests to show delayed or deranged neurobehavioural development.
These powerful epidemiological methods have enabled the discovery of additional developmental neurotoxicants.
Early-life exposures to neurotoxic chemicals
Development/programming
Functional maturation
Neurological disease and degenerative changes
Figure 1: Effect of neurotoxicants during early brain development Exposures in early life to neurotoxic chemicals can cause a wide range of adverse effects on brain development and maturation that can manifest as functional impairments or disease at any point in the human lifespan, from early infancy to very old age.
www.thelancet.com/neurology Vol 13 March 2014
Review
AB
Figure 2: Functional MRI scans show abnormal activation in the brain
Average activation during finger tapping with the left hand in three adolescents with increased prenatal methylmercury exposure (A) and three control adolescents (B). The control participants activate the premotor and motor cortices on the right, whereas participants exposed to methylmercury activate these areas bilaterally.31
Cross-sectional data from Bangladesh show that exposure to manganese from drinking water is associated with reduced mathematics achievement scores in school children.39 A study in Quebec, Canada, showed a strong correlation between manganese concentrations in hair and hyperactivity.40 School-aged children living near manganese mining and processing facilities have shown associations between airborne manganese concentrations and diminished intellectual function41 and with impaired motor skills and reduced olfactory function.42 These results are supported by experimental findings in mice.43
A meta-analysis of 27 cross-sectional studies of children exposed to fluoride in drinking water, mainly from China, suggests an average IQ decrement of about seven points in children exposed to raised fluoride concentrations.44 ♦ Confounding from other substances seemed unlikely in most of these studies. Further characterisation of the dose–response association would be desirable.
The occupational health literature45 suggests that solvents can act as neurotoxicants, but the identifi cation of individual responsible compounds is hampered by the complexity of exposures. In a French cohort study of 3000 children, investigators linked maternal occupational solvent exposure during pregnancy to defi cuts in behavioural assessment at 2 years of age.46 The data showed dose-related increased risks for hyperactivity and aggressive behaviour. One in every five mothers in this cohort reported solvent exposures in common jobs, such as nurse or other hospital employee, chemist, cleaner, hairdresser, and beautician. In Massachusetts, USA, follow-up of a well-defined population with prenatal and early childhood exposure to the solvent tetrachloroethylene (also called perchlor ethylene) in drinking water showed a tendency towards deficient neurological function and increased risk of psychiatric diagnoses.47
Acute pesticide poisoning occurs frequently in children worldwide, and subclinical pesticide toxicity is also widespread. Clinical data suggest that acute pesticide poisoning during childhood might lead to lasting neurobehavioural defi cits.48,49 Highly toxic and bioaccumulative pesticides are now banned in high-income nations, but are still used in many low-income and middle- income countries. In particular, the organochlorine compounds dichlorodiphenyltrichloroethane (DDT), its metabolite dichlorodiphenyldichloroethylene (DDE), and chlordecone (Kepone), tend to be highly persistent and remain widespread in the environment and in people’s bodies in high-use regions. Recent studies have shown inverse correlations between serum concentrations of DDT or DDE (which indicate accumulated exposures), and neurodevelopmental performance.50,51
Organophosphate pesticides are eliminated from the human body much more rapidly than are organochlorines, and exposure assessment is therefore inherently less precise. Nonetheless, three prospective epidemiological birth cohort studies provide new evidence that prenatal exposure to organophosphate pesticides can cause developmental neurotoxicity. In these studies, prenatal organophosphate exposure was assessed by measurement of maternal urinary excretion of pesticide metabolites during pregnancy. Dose-related correlations were recorded between maternal exposures to chlorpyrifos or other organophosphates and small head circumference at birth—which is an indication of slowed brain growth in utero—and with neurobehavioural deficits that have persisted to at least 7 years of age.52–54 In a subgroup study, MRI of the brain showed that prenatal chlorpyrifos exposure was associated with structural abnormalities that included thinning of the cerebral cortex.55
Herbicides and fungicides might also have neurotoxic potential.56 Propoxur,57 a carbamate pesticide, and permethrine,58 a member of the pyrethroid class of pesticides, have recently been linked to neuro developmental deficits in children.
The group of compounds known as polybrominated diphenyl ethers (PBDEs) are widely used as flame retardants and are structurally very similar to the polychlorinated biphenyls. Experimental evidence now suggests that the PBDEs might also be neurotoxic.59
Epidemiological studies in Europe and the USA have shown neurodevelopmental deficits in children with increased prenatal exposures to these compounds.60–62
Thus, the PBDEs should be regarded as hazards to human neurobehavioural development, although attribution of relative toxic potentials to individual PBDE congeners is not yet possible.
Other suspected developmental neurotoxicants
A serious difficulty that complicates many epidemiological studies of neurodevelopmental toxicity in children is the problem of mixed exposures. Most populations are exposed to more than one neurotoxicant at a time, and yet
332 www.thelancet.com/neurology Vol 13 March 2014
Review
most studies have only a finite amount of power and precision in exposure assessment to discern the possible effects of even single neurotoxicants. A further problem in many epi demiological studies of non-persistent toxicants is that imprecise assessment of exposure tends to obscure associations that might actually be present.63
Guidance from experimental neurotoxicity studies is therefore crucial. In the assessment of potential developmental neurotoxicants, we have used a strength of evidence approach similar to that used by the International Agency for Research on Cancer for assessing epidemiological and experimental studies. Phthalates and bisphenol A are added to many different types of plastics, cosmetics, and other consumer products. Since they are eliminated rapidly in urine, exposure assessment is complicated, and such imprecision might lead to underestimation of the true risk of neurotoxicity. The best-documented eff ects of early-life exposure to phthalates are the consequence of disruption of endocrine signalling.64 Thus, prenatal exposures to phthalates have been linked to both neurodevelopmental deficits and to behavioural abnormalities characterised by shortened attention span and impaired social interactions.65 The neurobehavioral toxicity of these compounds seems to affect mainly boys and could therefore relate to endocrine disruption in the developing brain.66 In regard to bisphenol A, a prospective study showed that point estimates of exposure during gestation were linked to abnormalities in behaviour and executive function in children at 3 years of age.67
Exposure to air pollution can cause neuro developmental delays and disorders of behavioural functions.68,69 Of the individual components of air pollution, carbon monoxide is a well-documented neurotoxicant, and indoor exposure to this substance has now been linked to defycient neurobehavioural performance in children.70 Less clear is the reported contribution of nitrogen oxides to neurodevelopmental defi cits,71 since these compounds often co-occur with carbon monoxide as part of complex emissions. Tobacco smoke is a complex mixture of hundreds of chemical compounds and is now a well- documented cause of developmental neurotoxicity.72
Infants exposed pre natally to polycyclic aromatic hydrocarbons from traffic exhausts at 5 years of age showed greater cognitive impairment and lower IQ than those exposed to lower levels of these compounds.68
Perfluorinated compounds, such as perfluorooctanoic acid and perfluorooctane sulphonate, are highly persistent in the environment and in the human body, and seem to be neurotoxic.73 Emerging epidemiological evidence suggests that these compounds might indeed impede neurobehavioural development.74
Developmental neurotoxicity and clinical neurology Exposures in early life to developmental neurotoxicants are now being linked to specific clinical syndromes in children. For example, an increased risk of attentiondeficit hyperactivity disorder has been linked to prenatal exposures to manganese, organophosphates,75 and phthalates.76 Phthalates have also been linked to behaviours that resemble components of autism spectrum disorder.77 Prenatal exposure to automotive air pollution in California, USA, has been linked to an increased risk for autism spectrum disorder.78
The persistent decrements in intelligence documented in children, adolescents, and young adults exposed in early life to neurotoxicants could presage the development of neurodegenerative disease later in life. Thus, accumulated exposure to lead is associated with cognitive decline in the elderly.79
Manganese exposure may lead to parkinsonism, and experimental studies have reported Parkinson’s disease as a result of developmental exposures to the insecticide rotenone, the herbicides paraquat and maneb, and the solvent trichloroethylene.80 Any environmental exposure that increases the risk of neurodegenerative disorders in later life (figure 1) requires urgent investigation as the world’s population continues to age.81
The expanding complement of neurotoxicants In our 2006 review,6 we expressed concern that additional developmental neurotoxicants might lie undiscovered in the 201 chemicals that were then known to be neurotoxic to human adults, in the roughly 1000 chemicals known to be neurotoxic in animal species, and in the many thousands of industrial chemicals and pesticides that have never been tested for neurotoxicity. Exposure to neurotoxic chemicals is not rare, since almost half of the 201 known human neurotoxicants are regarded as high production volume chemicals. Our updated literature review shows that since 2006 the list of recognised human neurotoxicants has expanded by 12 chemicals, from 202 (including ethanol) to 214 (table 1 and appendix)—that is, by about two substances per year. Many of these chemicals are widely used and disseminated extensively in the global environment. Of the newly identified neuro developmental toxicants, pesticides constitute the largest group, as was already the case
See Online for appendix
Number Number Identified since 2006
known in known in
2006 2013
Metals and inorganic 25 26 Hydrogen phosphide82
compounds Organic solvents 39* 40 Ethyl chloride83
Pesticides 92 101
Acetamiprid,84 amitraz,85 avermectin,86 emamectin,87
fipronil (Termidor), [FLUORIDE] 88 glyphosate,89 hexaconazole,90
imidacloprid,91 tetramethylenedisulfotetramine92
Other organic compounds 46 47 1,3-butadiene93
Total 202* 214 12 new substances
*Including ethanol.
Table 1: Industrial chemicals known to be toxic to the human nervous system in 2006 and 2013,
according to chemical group
www.thelancet.com/neurology Vol 13 March 2014
Review
Known in 2006 Newly identified
Metals and inorganic compounds Arsenic and arsenic compounds, Fluoride and manganese lead, and methylmercury Organic solvents (Ethanol) toluene Tetrachloroethylene
Pesticides None Chlorpyrifos and DDT/DDE
Other organic compounds Polychlorinated biphenyls Brominated diphenyl ethers
Total 6* 6
DDT=dichlorodiphenyltrichloroethane. DDE=dichlorodiphenyldichloroethylene. *Including ethanol.
Table 2: Industrial chemicals known to cause developmental neurotoxicity in human beings in 2006 and
2013, according to chemical group
Number of IQ points lost
Major medical and neurodevelopmental disorders
Preterm birth 34 031 025
Autism spectrum disorders 7 109 899
Paediatric bipolar disorder 8 164 080
Attention-defi cit hyperactivity disorder 16 799 400
Postnatal traumatic brain injury 5 827 300
Environmental chemical exposures
Lead 22 947 450
Methylmercury 1 590 000*
Organophosphate pesticides 16 899 488
Other neurotoxicants Unknown
IQ=intelligence quotient. Data from from Bellinger.94 *From Grandjean and
colleagues.95
Table 3: Total losses of IQ points in US children 0–5 years of age associated with major risk factors, including developmental exposure to industrial chemicals that cause neurotoxicity 2006. In the same 7-year period, the number of known developmental neurotoxicants has doubled from six to 12 (table 2). Although the pace of scientific discovery of new neurodevelopmental hazards is more rapid today than in the past, it is still slower than the identification of adult neurotoxicants.
The gap that exists between the number of substances known to be toxic to the adult brain and the smaller number known to be toxic to the much more vulnerable developing brain is unlikely to close in the near future.
This discrepancy is attributable to the fact that toxicity to the adult brain is usually discovered as a result of acute poisoning incidents, typically with a clear and immediate association between causative exposure and adverse effects, as occurs for workplace exposures or suicide attempts. By contrast, the recognition of developmental neurotoxicity relies on two sets of evidence collected at two different points in time: exposure data (often obtained from the mother during pregnancy), and data for the child’s postnatal neurobehavioural development (often obtained 5–10 years later). Because brain functions develop sequentially, the full effects of early neurotoxic damage might not become apparent until school age or beyond. The most reliable evidence of developmental neurotoxicity is obtained through prospective studies that include real-time recording of information about exposure in early life followed by serial clinical assessments of the child. Such research is inherently slow and is hampered by the difficulty of reliable assessment of exposures to individual toxicants in complex mixtures.
Consequences of developmental neurotoxicity
Developmental neurotoxicity causes brain damage that is too often untreatable and frequently permanent. The consequence of such brain damage is impaired CNS function that lasts a lifetime and might result in reduced intelligence, as expressed in terms of lost IQ points, or disruption in behaviour. A recent study compared the estimated total IQ losses from major paediatric causes and showed that the magnitude of losses attributable to lead, pesticides, and other neurotoxicants was in the same range as, or even greater than, the losses associated with medical events such as preterm birth, traumatic brain injury, brain tumours, and congenital heart disease (table 3).94
Loss of cognitive skills reduces children’s academic and economic attainments and has substantial long-term economic effects on societies.4 Thus, each loss of one IQ point has been estimated to decrease average lifetime earnings capacity by about €12 000 or US$18 000 in 2008 currencies.96 The most recent estimates from the USA indicate that the annual costs of childhood lead poisoning are about US$50 billion and that the annual costs of methylmercury toxicity are roughly US$5 billion.97 In the European Union, methylmercury exposure is estimated to cause a loss of about 600 000 IQ points every year, corresponding to an annual economic loss of close to €10 billion. In France alone, lead exposure is associated with IQ losses that correspond to annual costs that might exceed €20 billion.98 Since IQ losses represent only one aspect of developmental neurotoxicity, the total costs are surely even higher.
Evidence from worldwide sources indicates that average national IQ scores are associated with gross domestic product (GDP)—a correlation that might be causal in both directions.99 Thus, poverty can cause low IQ, but the opposite is also true. In view of the widespread exposures to lead, pesticides, and other neurotoxicants in developing countries, where chemical controls might be ineffective compared with those in more developed countries,100,101 developmental exposures to industrial chemicals could contribute substantially to the recorded correlation between IQ and GDP. If this theory is true, developing countries could take decades to emerge from poverty. Consequently, pollution abatement might then be delayed, and a vicious circle can result.
The antisocial behaviour, criminal behaviour, violence, and substance abuse that seem to result from early-life exposures to some neurotoxic chemicals result in increased needs for special educational services, institutionalisation, and even incarceration. In the USA, the murder rate fell sharply 20 years after the removal of lead from petrol,102 a finding consistent with the idea that 334
www.thelancet.com/neurology Vol 13 March 2014
Review
exposure to lead in early life is a powerful determinant of behaviour decades later. Although poorly quantified, such behavioural and social consequences of neuro-development toxicity are potentially very costly.76
Prevention of developmental neurotoxicity caused by industrial chemicals is highly cost effective. A study that quantified the gains resulting from the phase-out of lead additives from petrol reported that in the USA alone, the introduction of lead-free petrol has generated an economic benefit of $200 billion in each annual birth cohort since 1980,103 an aggregate benefit in the past 30 years of over $3 trillion. This success has since been repeated in more than 150 countries, resulting in vast additional savings.
Every US$1 spent to reduce lead hazards is estimated to produce a benefit of US$17–220, which represents a cost- benefit ratio that is even better than that for vaccines.4 Furthermore, the costs associated with the late-life consequences of developmental neurotoxicity are enormous, and the benefits from prevention of degenerative brain disorders could be very substantial.
New methods to identify developmental neurotoxicants
New toxicological methods now allow a rational strategy for the identification of developmental neurotoxicants based on a multidisciplinary approach.104 A new guideline has been approved as a standardised approach for the identification of developmental neurotoxicants.105
However, completion of such tests is expensive and requires the use of many laboratory animals, and reliance on mammals for chemicals testing purposes needs to be reduced.106 US governmental agencies have established the National Center for Computational Toxicology and an initiative— the Tox 21 Program—to promote the evolution of toxicology from a mainly observational science to a predominantly predictive science.107
In-vitro methods have now reached a level of predictive validity that means they can be applied to neurotoxicity testing.108 Some of these tests are based on neural stem cells. Although these cell systems do not have a blood– brain barrier and particular metabolising enzymes, these approaches are highly promising. As a further option, data for protein links and protein–protein interactions can now be used to explore potential neurotoxicity in silica, 109 thus showing that existing computational methods might predict potential toxic eff ects.110 In summary, use of the whole range of approaches along with clinical and epidemiological evidence, when available, should enable the integration of information for use in at least a tentative risk assessment. With these methods, we anticipate that the pace of scientifi c discovery in developmental neurotoxicology will accelerate further in the years ahead.
Conclusions and Recommendations
The updated findings presented in this Review confirm and extend our 2006 conclusions.6 During the 7 years since our previous report, the number of industrial chemicals recognised to be developmental neurotoxicants has doubled. Exposures to these industrial chemicals in the environment contribute to the pandemic of developmental neurotoxicity.
Two major obstacles impede efforts to control the global pandemic of developmental neurotoxicity. These barriers, which we noted in our previous review 6 and were recently underlined by the US National Research Council,111 are: large gaps in the testing of chemicals for developmental neurotoxicity, which results in a paucity of systematic data to guide prevention; and the huge amount of proof needed for regulation. Thus, very few chemicals have been regulated as a result of developmental neurotoxicity.
The presumption that new chemicals and technologies are safe until proven otherwise is a fundamental problem.111 Classic examples of new chemicals that were introduced because they conveyed certain benefits, but were later shown to cause great harm, include several neurotoxicants, asbestos, thalidomide, diethylstilbestrol, and the chlorofluorocarbons.112 A recurring theme in each of these cases was that commercial introduction and wide dissemination of the chemicals preceded any systematic effort to assess potential toxicity. Particularly absent were advance efforts to study possible effects on children’s health or the potential of exposures in early life to disrupt early development. Similar challenges have been confronted in other public health disasters, such as those caused by tobacco smoking, alcohol use, and refined foods. These problems have been recently termed industrial epidemics.113
To control the pandemic of developmental neurotoxicity, we propose a coordinated international strategy (panel).
Mandatory and transparent assessment of evidence for neurotoxicity is the foundation of this strategy.
Assessment of toxicity must be followed by governmental regulation and market intervention. Voluntary controls seem to be of little value.11
Panel: Recommendations for an international clearinghouse on neurotoxicity The main purpose of this agency would be to promote optimum brain health, not just avoidance of neurological disease, by inspiring, facilitating, and coordinating research and public policies that aim to protect brain development during the most sensitive life stages.
The main efforts would aim to:
Screen industrial chemicals present in human exposures for neurotoxic effects so that
hazardous substances can be identified for tighter control.
Stimulate and coordinate new research to understand how toxic chemicals interfere with brain development and how best to prevent long-term dysfunctions and deficits
•Function as a clearinghouse for research data and strategies by gathering and assessing documentation about brain toxicity and stimulating international collaboration on research and prevention
•Promote policy development aimed at protecting vulnerable populations against chemicals that are toxic to the brain without needing unrealistic amounts of scientific proof www.thelancet.com/neurology Vol 13 March 2014
Review
The three pillars of our proposed strategy are:
legally mandated testing of existing industrial chemicals and pesticides already in commerce, with prioritisation of those with the most widespread use, and incorporation of new assessment technologies; legally mandated premarket evaluation of new chemicals before they enter markets, with use of precautionary approaches for chemical testing that recognise the unique vulnerability of the developing brain; and the formation of a new clearinghouse for neurotoxicity as a parallel to the International Agency for Research on Cancer. This new agency will assess industrial chemicals for developmental neurotoxicity with a precautionary approach that emphasises prevention and does not require absolute proof of toxicity. It will facilitate and coordinate epidemiological and toxicological studies and will lead the urgently needed global programmes for prevention.
These new approaches must reverse the dangerous presumption that new chemicals and technologies are safe until proven otherwise. They must also overcome the existing requirement to produce absolute proof of toxicity before action can be started to protect children against neurotoxic substances. Precautionary interpretation of data about developmental neurotoxicity should take into account the very large individual and societal costs that result from failure to act on available documentation to prevent disease in children.114 Academic research has often favoured scepticism and required extensive replication before acceptance of a hypothesis,114 thereby adding to the inertia in toxicology and environmental health research and the consequent disregard of many other potential neurotoxicants.115 Additionally, the strength of evidence that is needed to constitute “proof” should be analysed in a societal perspective, so that the implications of ignoring a developmental neurotoxicant and of failing to act on the basis of available data are also taken into account.
Finally, we emphasise that the total number of neurotoxic substances now recognised almost certainly represents an underestimate of the true number of developmental neurotoxicants that have been released into the global environment. Our very great concern is that children [?]
Search strategy and selection criteria We identified studies published since 2006 on the neurotoxic effects of industrial chemicals in human beings by using the search terms “neurotoxicity syndromes”[MeSH], “neurotoxic”,“neurologic”, or “neuro*”, combined with “exposure” and “poisoning” in PubMed, from 2006 to the end of 2012. For developmental neurotoxicity, the search terms were “prenatal exposure delayed effects”[MeSH], “maternal exposure” or “maternal fetal exchange”, “developmental disabilities/chemically induced” and “neurotoxins”, all of which were searched for with the limiters “All Child: 0–18 years, Human”.
We also used references cited in the publications retrieved. worldwide are being exposed to unrecognised toxic chemicals that are silently eroding intelligence, disrupting behaviours, truncating future achievements, and damaging societies, perhaps most seriously in developing countries. A new framework of action is needed.
Contributors
Both authors did the literature review, wrote and revised the report, and approved the final version.
Conflicts of interest
PG has provided paid expert testimony about mercury toxicology for the US Department of Justice. PJL has provided paid expert testimony in cases of childhood lead poisoning. We declare that we have no other conflicts of interest.
Acknowledgments
This work was supported by the National Institutes of Health, National Institute for Environmental Health Sciences (ES09584, ES09797, and ES11687). The funding source had no role in the literature review, interpretation of data, writing of this Review, or in the decision to submit for publication. The contents of this paper are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health. We thank Mary S Wolff (Icahn School of Medicine at Mount Sinai, New York, NY, USA) and Linda S Birnbaum (US National Institute of Environmental Health Sciences, Research Triangle Park, NC, USA) for their critical reading of the report.
References
1
Bloom B, Cohen RA, Freeman G. Summary health statistics
for U.S. children: National Health Interview Survey, 2009.
Vital Health Stat 2010; 10: 1–82.
2
Landrigan PJ, Lambertini L, Birnbaum LS. A research strategy to
discover the environmental causes of autism and neurodevelopmental
disabilities. Environ Health Perspect 2012; 120: a258–60.
3
Bellinger DC. Interpreting epidemiologic studies of developmental
neurotoxicity: conceptual and analytic issues. Neurotoxicol Teratol
2009; 31: 267–74.
4
Gould E. Childhood lead poisoning: conservative estimates of the
social and economic benefits of lead hazard control.
Environ Health Perspect 2009; 117: 1162–67.
5
National Research Council. Scientific frontiers in developmental
toxicology and risk assessment. Washington, DC: National
Academies Press, 2000.
6
Grandjean P, Landrigan PJ. Developmental neurotoxicity of
industrial chemicals. Lancet 2006; 368: 2167–78.
7
Grandjean P. Only one chance. How environmental pollution
impairs brain development – and how to protect the brains of the
next generation. New York: Oxford University Press, 2013.
8
Rice D, Barone S Jr. Critical periods of vulnerability for the
developing nervous system: evidence from humans and animal
models. Environ Health Perspect 2000; 108 (suppl 3): 511–33.
9
Needleman HL. The removal of lead from gasoline: historical and
personal reflections. Environ Res 2000; 84: 20–35.
10
Grandjean P, Satoh H, Murata K, Eto K. Adverse eff ects of
methylmercury: environmental health research implications.
Environ Health Perspect 2010; 118: 1137–45.
11
Landrigan PJ, Goldman LR. Children’s vulnerability to toxic
chemicals: a challenge and opportunity to strengthen health and
environmental policy. Health Aff 2011; 30: 842–50.
12
Weiss B. Food additives and environmental chemicals as sources of
childhood behavior disorders. J Am Acad Child Psychiatry 1982;
21: 144–52.
13 Needham LL, Grandjean P, Heinzow B, et al. Partition of
environmental chemicals between maternal and fetal blood and
tissues. Environ Sci Technol 2011; 45: 1121–26.
14 Environmental Working Group. Body burden—the pollution in
newborns. Washington, DC: Environmental Working Group, 2005.
15 Zheng W, Aschner M, Ghersi-Egea JF. Brain barrier systems: a new
frontier in metal neurotoxicological research. Toxicol Appl Pharmacol
2003; 192: 1–11.
16 Bose R, Onishchenko N, Edoff K, Janson Lang AM, Ceccatelli S.
Inherited effects of low-dose exposure to methylmercury in neural
stem cells. Toxicol Sci 2012; 130: 383–90.
336
www.thelancet.com/neurology Vol 13 March 2014
Review
7 Costa LG. Current issues in organophosphate toxicology.
Clin Chim Acta 2006; 366: 1–13.
18 Augusti-Tocco G, Biagioni S, Tata AM. Acetylcholine and regulation of
gene expression in developing systems. J Mol Neurosci 2006; 30: 45–48.
19 Roth TL. Epigenetics of neurobiology and behavior during
development and adulthood. Dev Psychobiol 2012; 54: 590–97.
20
Lanphear BP, Hornung R, Khoury J, et al. Low-level environmental
lead exposure and children’s intellectual function: an international
pooled analysis. Environ Health Perspect 2005; 113: 894–99.
21
Budtz-Jorgensen E, Bellinger D, Lanphear B, Grandjean P.
An international pooled analysis for obtaining a benchmark dose for
environmental lead exposure in children. Risk Anal 2013; 33: 450–61.
22
Grandjean P. Even low-dose lead exposure is hazardous. Lancet
2010; 376: 855–56.
23
Mazumdar M, Bellinger DC, Gregas M, Abanilla K, Bacic J,
Needleman HL. Low-level environmental lead exposure in childhood
and adult intellectual function: a follow-up study. Environ Health
2011; 10: 24.
24
Cecil KM, Brubaker CJ, Adler CM, et al. Decreased brain volume in
adults with childhood lead exposure. PLoS Med 2008; 5: e112.
25
Zhang N, Baker HW, Tufts M, Raymond RE, Salihu H, Elliott MR.
Early childhood lead exposure and academic achievement: evidence
from Detroit public schools, 2008–2010. Am J Public Health 2013;
103: e72–77.
26 Fergusson DM, Boden JM, Horwood LJ. Dentine lead levels in
childhood and criminal behaviour in late adolescence and early
adulthood. J Epidemiol Community Health 2008; 62: 1045–50.
27 Wright JP, Dietrich KN, Ris MD, et al. Association of prenatal and
childhood blood lead concentrations with criminal arrests in early
adulthood. PLoS Med 2008; 5: e101.
28 Oken E, Bellinger DC. Fish consumption, methylmercury and child
neurodevelopment. Curr Opin Pediatr 2008; 20: 178–83.
29 Debes F, Budtz-Jorgensen E, Weihe P, White RF, Grandjean P.
Impact of prenatal methylmercury exposure on neurobehavioral
function at age 14 years. Neurotoxicol Teratol 2006; 28: 536–47.
30 Julvez J, Smith GD, Golding J, et al. Genetic predisposition to
cognitive deficit at age 8 years associated with prenatal
methylmercury exposure. Epidemiology 2013; 24: 643–50.
31 White RF, Palumbo CL, Yurgelun-Todd DA, et al. Functional MRI
approach to developmental methylmercury and polychlorinated
biphenyl neurotoxicity. Neurotoxicology 2011; 32: 975–80.
32 Budtz-Jorgensen E, Grandjean P, Weihe P. Separation of risks and
benefits of seafood intake. Environ Health Perspect 2007; 115: 323–27.
33 Strain JJ, Davidson PW, Bonham MP, et al. Associations of
maternal long-chain polyunsaturated fatty acids, methyl mercury,
and infant development in the Seychelles Child Development
Nutrition Study. Neurotoxicology 2008; 29: 776–82.
34 Wasserman GA, Liu X, Parvez F, et al. Water arsenic exposure and
intellectual function in 6-year-old children in Araihazar,
Bangladesh. Environ Health Perspect 2007; 115: 285–89.
35 Hamadani JD, Tofail F, Nermell B, et al. Critical windows of
exposure for arsenic-associated impairment of cognitive function in
pre-school girls and boys: a population-based cohort study.
Int J Epidemiol 2011; 40: 1593–604.
36 Tanaka H, Tsukuma H, Oshima A. Long-term prospective study of
6104 survivors of arsenic poisoning during infancy due to
contaminated milk powder in 1955. J Epidemiol 2010; 20: 439–45.
37 Engel SM, Wolff MS. Causal inference considerations for endocrine
disruptor research in children’s health. Annu Rev Public Health
2013; 34: 139–58.
38 Mattson SN, Crocker N, Nguyen TT. Fetal alcohol spectrum
disorders: neuropsychological and behavioral features.
Neurospychol Rev 2011; 21: 81–101.
39 Khan K, Wasserman GA, Liu X, et al. Manganese exposure from
drinking water and children’s academic achievement.
Neurotoxicology 2012; 33: 91–97.
40 Bouchard M, Laforest F, Vandelac L, Bellinger D, Mergler D. Hair
manganese and hyperactive behaviors: pilot study of school-age
children exposed through tap water. Environ Health Perspect 2007;
115: 122–27.
41 Riojas-Rodriguez H, Solis-Vivanco R, Schilmann A, et al.
Intellectual function in Mexican children living in a mining area
and environmentally exposed to manganese. Environ Health Perspect
2010; 118: 1465–70.
42
Lucchini RG, Guazzetti S, Zoni S, et al. Tremor, olfactory and
motor changes in Italian adolescents exposed to historical
ferro-manganese emission. Neurotoxicology 2012; 33: 687–96.
43
Moreno JA, Yeomans EC, Streifel KM, Brattin BL, Taylor RJ,
Tjalkens RB. Age-dependent susceptibility to manganese-induced
neurological dysfunction. Toxicol Sci 2009; 112: 394–404.
44
Choi AL, Sun G, Zhang Y, Grandjean P. Developmental fl uoride
neurotoxicity: a systematic review and meta-analysis.
Environ Health Perspect 2012; 120: 1362–68.
45
Julvez J, Grandjean P. Neurodevelopmental toxicity risks due to
occupational exposure to industrial chemicals during pregnancy.
Ind Health 2009; 47: 459–68.
46
Pele F, Muckle G, Costet N, et al. Occupational solvent exposure
during pregnancy and child behaviour at age 2. Occup Environ Med
2013; 70: 114–19.
47
Janulewicz PA, White RF, Martin BM, et al. Adult
neuropsychological performance following prenatal and early
postnatal exposure to tetrachloroethylene (PCE)-contaminated
drinking water. Neurotoxicol Teratol 2012; 34: 350–59.
48
Kofman O, Berger A, Massarwa A, Friedman A, Jaffar AA. Motor
inhibition and learning impairments in school-aged children
following exposure to organophosphate pesticides in infancy.
Pediatr Res 2006; 60: 88–92.
49
London L, Beseler C, Bouchard MF, et al. Neurobehavioral and
neurodevelopmental effects of pesticide exposures. Neurotoxicology
2012; 33: 887–96.
50
Torres-Sanchez L, Schnaas L, Rothenberg SJ, et al. Prenatal
p,p’-DDE exposure and neurodevelopment among children
3.5–5 years of age. Environ Health Perspect 2013; 121: 263–68.
51
Boucher O, Simard MN, Muckle G, et al. Exposure to an
organochlorine pesticide (chlordecone) and development of
18-month-old infants. Neurotoxicology 2013; 35: 162–68.
52
Rauh V, Arunajadai S, Horton M, et al. 7-year neurodevelopmental
scores and prenatal exposure to chlorpyrifos, a common agricultural
pesticide. Environ Health Perspect 2011; 119: 1196–201.
53
Bouchard MF, Chevrier J, Harley KG, et al. Prenatal exposure to
organophosphate pesticides and IQ in 7-year old children.
Environ Health Perspect 2011; 119: 1189–95.
54
Engel SM, Wetmur J, Chen J, et al. Prenatal exposure to
organophosphates, paraoxonase 1, and cognitive development in
childhood. Environ Health Perspect 2011; 119: 1182–88.
55
Rauh VA, Perera FP, Horton MK, et al. Brain anomalies in children
exposed prenatally to a common organophosphate pesticide.
Proc Natl Acad Sci USA 2012; 109: 7871–76.
56
Bjorling-Poulsen M, Andersen HR, Grandjean P. Potential
developmental neurotoxicity of pesticides used in Europe.
Environ Health 2008; 7: 50.
57
Ostrea EM Jr, Reyes A, Villanueva-Uy E, et al. Fetal exposure to
propoxur and abnormal child neurodevelopment at 2 years of age.
Neurotoxicology 2012; 33: 669–75.
58
Horton MK, Rundle A, Camann DE, Boyd Barr D, Rauh VA,
Whyatt RM. Impact of prenatal exposure to piperonyl butoxide and
permethrin on 36-month neurodevelopment. Pediatrics 2011;
127: e699–706.
59 Dingemans MM, van den Berg M, Westerink RH. Neurotoxicity of
brominated flame retardants: (in)direct effects of parent and
hydroxylated polybrominated diphenyl ethers on the (developing)
nervous system. Environ Health Perspect 2011; 119: 900–07.
60 Roze E, Meijer L, Bakker A, Van Braeckel KN, Sauer PJ, Bos AF.
Prenatal exposure to organohalogens, including brominated fl ame
retardants, influences motor, cognitive, and behavioral
performance at school age. Environ Health Perspect 2009;
117: 1953–58.
61
Herbstman JB, Sjodin A, Kurzon M, et al. Prenatal exposure to
PBDEs and neurodevelopment. Environ Health Perspect 2010;
118: 712–19.
62 Eskenazi B, Chevrier J, Rauch SA, et al. In utero and childhood
polybrominated diphenyl ether (PBDE) exposures and
neurodevelopment in the CHAMACOS study.
Environ Health Perspect 2013; 121: 257–62.
63 Grandjean P, Budtz-Jorgensen E. An ignored risk factor in
toxicology: the total imprecision of exposure assessment.
Pure Appl Chem 2010; 82: 383–91.
www.thelancet.com/neurology Vol 13 March 2014
Review
64
Vandenberg LN, Colborn T, Hayes TB, et al. Hormones and
endocrine-disrupting chemicals: low-dose eff ects and
nonmonotonic dose responses. Endocr Rev 2012; 33: 378–455.
65
Engel SM, Miodovnik A, Canfield RL, et al. Prenatal phthalate
exposure is associated with childhood behavior and executive
functioning. Environ Health Perspect 2010; 118: 565–71.
66
Swan SH, Liu F, Hines M, et al. Prenatal phthalate exposure and
reduced masculine play in boys. Int J Androl 2010; 33: 259–69.
67
Braun JM, Kalkbrenner AE, Calafat AM, et al. Impact of early-life
bisphenol A exposure on behavior and executive function in
children. Pediatrics 2011; 128: 873–82.
68
Perera FP, Li Z, Whyatt R, et al. Prenatal airborne polycyclic
aromatic hydrocarbon exposure and child IQ at age 5 years.
Pediatrics 2009; 124: e195–202.
69
Calderon-Garciduenas L, Mora-Tiscareno A, Ontiveros E, et al. Air
pollution, cognitive deficits and brain abnormalities: a pilot study
with children and dogs. Brain Cogn 2008; 68: 117–27.
70
Dix-Cooper L, Eskenazi B, Romero C, Balmes J, Smith KR.
Neurodevelopmental performance among school age children in
rural Guatemala is associated with prenatal and postnatal exposure
to carbon monoxide, a marker for exposure to woodsmoke.
Neurotoxicology 2012; 33: 246–54.
71
Vrijheid M, Martinez D, Aguilera I, et al. Indoor air pollution from gas
cooking and infant neurodevelopment. Epidemiology 2012; 23: 23–32.
72
Hernandez-Martinez C, Arija Val V, Escribano Subias J,
Canals Sans J. A longitudinal study on the effects of maternal
smoking and secondhand smoke exposure during pregnancy on
neonatal neurobehavior. Early Hum Dev 2012; 88: 403–08.
73
Mariussen E. Neurotoxic effects of perfl uoroalkylated compounds:
mechanisms of action and environmental relevance. Arch Toxicol
2012; 86: 1349–67.
74
Gump BB, Wu Q, Dumas AK, Kannan K. Perfl uorochemical (PFC)
exposure in children: associations with impaired response
inhibition. Environ Sci Technol 2011; 45: 8151–59.
75
Froehlich TE, Anixt JS, Loe IM, Chirdkiatgumchai V, Kuan L,
Gilman RC. Update on environmental risk factors for attentiondefi
cit/hyperactivity disorder. Curr Psychiatry Rep 2011; 13: 333–44.
76
Carpenter DO, Nevin R. Environmental causes of violence.
Physiol Behav 2010; 99: 260–68.
77
Miodovnik A, Engel SM, Zhu C, et al. Endocrine disruptors and
childhood social impairment. Neurotoxicology 2011; 32: 261–67.
78
Volk HE, Lurmann F, Penfold B, Hertz-Picciotto I, McConnell R.
Traffic-related air pollution, particulate matter, and autism.
JAMA Psychiatry 2013; 70: 71–77.
79
Bandeen-Roche K, Glass TA, Bolla KI, Todd AC, Schwartz BS.
Cumulative lead dose and cognitive function in older adults.
Epidemiology 2009; 20: 831–39.
80
Lock EA, Zhang J, Checkoway H. Solvents and Parkinson disease:
a systematic review of toxicological and epidemiological evidence.
Toxicol Appl Pharmacol 2013; 266: 345–55.
81
Landrigan PJ, Sonawane B, Butler RN, Trasande L, Callan R,
Droller D. Early environmental origins of neurodegenerative
disease in later life. Environ Health Perspect 2005; 113: 1230–33.
82
Lauterbach M, Solak E, Kaes J, Wiechelt J, Von Mach MA,
Weilemann LS. Epidemiology of hydrogen phosphide exposures in
humans reported to the poison center in Mainz, Germany,
1983–2003. Clin Toxicol 2005; 43: 575–81
83
Demarest C, Torgovnick J, Sethi NK, Arsura E, Sethi PK. Acute
reversible neurotoxicity associated with inhalation of ethyl chloride:
a case report. Clin Neurol Neurosurg 2011; 113: 909–10.
84
Imamura T, Yanagawa Y, Nishikawa K, Matsumoto N, Sakamoto T.
Two cases of acute poisoning with acetamiprid in humans.
Clin Toxicol 2010; 48: 851–53.
85
Veale DJ, Wium CA, Muller GJ. Amitraz poisoning in South Africa:
a two year survey (2008–2009). Clin Toxicol 2011; 49: 40–44.
86
Sung YF, Huang CT, Fan CK, Lin CH, Lin SP. Avermectin
intoxication with coma, myoclonus, and polyneuropathy. Clin Toxicol
2009; 47: 686–88.
87
Yang CC. Acute human toxicity of macrocyclic lactones.
Curr Pharm Biotechnol 2012; 13: 999–1003.
88
Lee SJ, Mulay P, Diebolt-Brown B, et al. Acute illnesses associated
with exposure to fipronil—surveillance data from 11 states in the
United States, 2001–2007. Clin Toxicol 2010; 48: 737–44.
89
Malhotra RC, Ghia DK, Cordato DJ, Beran RG. Glyphosate surfactant
herbicide-induced reversible encephalopathy.
J Clin Neurosci 2010; 17: 1472–73.
90
David D, Prabhakar A, Peter JV, Pichamuthu K. Human poisoning
with hexastar: a hexaconazole-containing agrochemical fungicide.
Clin Toxicol 2008; 46: 692–93.
91
Shadnia S, Moghaddam HH. Fatal intoxication with imidacloprid
insecticide. Am J Emerg Med 2008; 26: 634.e1–4.
92
Deng X, Li G, Mei R, Sun S. Long term effects of tetramine
poisoning: an observational study. Clin Toxicol 2012; 50: 172–75.
93
Khalil M, Abudiab M, Ahmed AE. Clinical evaluation of 1,3-butadiene
neurotoxicity in humans. Toxicol Ind Health 2007; 23: 141–46.
94
Bellinger DC. A strategy for comparing the contributions of
environmental chemicals and other risk factors to neurodevelopment
of children. Environ Health Perspect 2012; 120: 501–07.
95
Grandjean P, Pichery C, Bellanger M, Budtz-Jorgensen E.
Calculation of mercury’s effects on neurodevelopment.
Environ Health Perspect 2012; 120: A452.
96
Bellanger M, Pichery C, Aerts D, et al. Economic benefi ts of
methylmercury exposure control in Europe: monetary value of
neurotoxicity prevention. Environ Health 2013; 12: 3.
97
Trasande L, Liu Y. Reducing the staggering costs of environmental
disease in children, estimated at $76.6 billion in 2008. Health Aff
2011; 30: 863–70.
98
Pichery C, Bellanger M, Zmirou-Navier D, Glorennec P,
Hartemann P, Grandjean P. Childhood lead exposure in France:
benefit estimation and partial cost-benefit analysis of lead hazard
control. Environ Health 2011; 10: 44.
99
Lynn R, Vanhanen T. IQ and the wealth of nations. Westport:
Praeger, 2002.
100 Blacksmith Institute. The world’s worst pollution problems:
assessing health risks at hazardous waste sites. New York:
Blacksmith Institute, 2012.
101
Trasande L, Massey RI, DiGangi J, Geiser K, Olanipekun AI,
Gallagher L. How developing nations can protect children from
hazardous chemical exposures while sustaining economic growth.
Health Aff 2011; 30: 2400–09.
102 Nevin R. Understanding international crime trends: the legacy of
preschool lead exposure. Environ Res 2007; 104: 315–36.
103 Schwartz J. Societal benefits of reducing lead exposure. Environ Res
1994; 66: 105–24.
104
National Research Council. Toxicity testing in the 21st century: a vision
and a strategy. Washington, DC: National Academies Press, 2007.
105 Makris SL, Raffaele K, Allen S, et al. A retrospective performance
assessment of the developmental neurotoxicity study in support of
OECD test guideline 426. Environ Health Perspect 2009; 117: 17–25.
106 Rovida C, Longo F, Rabbit RR. How are reproductive toxicity and
developmental toxicity addressed in REACH dossiers? Altex 2011;
28: 273–94.
107 Collins FS, Gray GM, Bucher JR. Toxicology. Transforming
environmental health protection. Science 2008; 319: 906–07.
108 Crofton KM, Mundy WR, Lein PJ, et al. Developmental neurotoxicity
testing: recommendations for developing alternative methods for the
screening and prioritization of chemicals. Altex 2011; 28: 9–15.
109 Audouze K, Grandjean P. Application of computational systems
biology to explore environmental toxicity hazards.
Environ Health Perspect 2011; 119: 1754–59.
110 Willighagen EL, Jeliazkova N, Hardy B, Grafstrom RC, Spjuth O.
Computational toxicology using the OpenTox application
programming interface and Bioclipse. BMC Res Notes 2011; 4: 487.
111 National Research Council. Science and decisions: advancing risk
assessment. Washington, DC: National Academies Press, 2009.
112 Late lessons from early warnings: science, precaution, innovation.
Copenhagen: European Environment Agency, 2013.
113 Moodie R, Stuckler D, Monteiro C, et al. Profits and pandemics:
prevention of harmful effects of tobacco, alcohol, and ultra-
processed food and drink industries. Lancet 2013; 381: 670–79.
114 Grandjean P. Seven deadly sins of environmental epidemiology and
the virtues of precaution. Epidemiology 2008; 19: 158–62.
115 Grandjean P, Eriksen ML, Ellegaard O, Wallin JA. The Matthew
effect in environmental science publication: a bibliometric analysis of
chemical substances in journal articles. Environ Health 2011; 10: 96.
338
www.thelancet.com/neurology Vol 13 March 2014
♦ + ItQ decrement of about seven points for each sucessive generation.
MORE INFO → HERE
IT’S INDEPENDENCE DAY !
As from today, water fluoridation must be prohibited in all Member States of the EC
Doug Cross
20th January 2014
(For the PDF version of this comment CLICK HERE )
The last legal loophole through which the British and Irish governments have been able to wriggle in their continued imposition of fluoridated water supplies finally closed today. The addition of fluorosilicic acid to any food is now completely banned throughout the entire European Community.
June 2013
This is not a recent event but seems to have been missed by the main media.
7 October 2012
Fluoride Accident South Korea
↓ This Video runs for 65 seconds ↓
Hydrogen Fluoride kills 5
↑ Warning, a disturbing short video ↑
An estimated 8 tons of HF was released.
5 people including the 2 workers perished,
18 responders, workers, reporter wound-up in the hospital,
almost 3000 villagers from 2 villages downwind of the facility
were treated for irritation, exposure.
Five workers were killed and 18 others were injured in the blast at chemical maker Hube Global at the Gumi National Industrial Complex in the industrial city, about 200 kilometers southeast of Seoul. The gas leak has cost factories in the industrial complex about 17.7 billion won (US$15.9 million) in lost production, officials said. Hundreds of angry villagers in Gumi who suffered after the massive gas leak moved to a safer region with some residents reporting blood in their saliva. About 110 elderly people in Bongsan-ri village evacuated to a facility about 10 kilometers away.
We are sorry if this is a bit technical …
Developmental Fluoride Neurotoxicity:
A Systematic Review and Meta-Analysis
Anna L. Choi,1 Guifan Sun,2 Ying Zhang,3 and Philippe Grandjean1,4
Author information ► Article notes ►
Copyright and License information ►
Abstract
Background:
Although fluoride may cause neurotoxicity in animal models and
acute fluoride poisoning causes neurotoxicity in adults,
very little is known of its effects on children’s neurodevelopment.
Objective:
We performed a systematic review and meta-analysis of published studies to investigatethe effects of increased fluoride exposure and delayed neurobehavioral development.Methods: We searched the MEDLINE, EMBASE, Water Resources Abstracts, and TOXNET databases through 2011 for eligible studies. We also searched the China National Knowledge Infrastructure (CNKI) database, because many studies on fluoride neurotoxicity have been published in Chinese journals only. In total, we identified 27 eligible epidemiological studies with high and reference exposures, end points of IQ scores, or related cognitive function measures with means and variances for the two exposure groups. Using random-effects models, we estimated the standardized mean difference between exposed and reference groups across all studies. We conducted sensitivity analyses restricted to studies using the same outcome assessment and having drinking-water fluoride as the only exposure. We performed the Cochran test for heterogeneity between studies, Begg’s funnel plot, and Egger test to assess publication bias, and conducted meta-regressions to explore sources of variation in mean differences among the studies.
Results:
The standardized weighted mean difference in IQ score between exposed and reference populations was –0.45 (95% confidence interval: –0.56, –0.35) using a random-effects model. Thus, children in high-fluoride areas had significantly lower IQ scores than those who lived in low-fluoride areas. Subgroup and sensitivity analyses also indicated inverse associations, although the substantial heterogeneity did not appear to decrease.
Conclusions:
The results support the possibility of an adverse effect of high fluoride exposure on children’s neurodevelopment. Future research should include detailed individual-level information on prenatal exposure, neurobehavioral performance, and covariates for adjustment.
Keywords:
fluoride, intelligence, neurotoxicityA recent report from the National Research Council (NRC 2006) concluded that adverse effects of high fluoride concentrations in drinking water may be of concern and that additional research is warranted. Fluoride may cause neurotoxicity in laboratory animals, including effects on learning and memory (Chioca et al. 2008; Mullenix et al. 1995). A recent experimental study where the rat hippocampal neurons were incubated with various concentrations (20 mg/L, 40 mg/L, and 80 mg/L) of sodium fluoride in vitro showed that fluoride neurotoxicity may target hippocampal neurons (Zhang M et al. 2008). Although acute fluoride poisoning may be neurotoxic to adults, most of the epidemiological information available on associations with children’s neurodevelopment is from China, where fluoride generally occurs in drinking water as a natural contaminant, and the concentration depends on local geological conditions. In many rural communities in China, populations with high exposure to fluoride in local drinking-water sources may reside in close proximity to populations without high exposure (NRC 2006). Opportunities for epidemiological studies depend on the existence of comparable population groups exposed to different levels of fluoride from drinking water. Such circumstances are difficult to find in many industrialized countries, because fluoride concentrations in community water are usually no higher than 1 mg/L, even when fluoride is added to water supplies as a public health measure to reduce tooth decay. Multiple epidemiological studies of developmental fluoride neurotoxicity were conducted in China because of the high fluoride concentrations that are substantially above 1 mg/L in well water in many rural communities, although microbiologically safe water has been accessible to many rural households as a result of the recent 5-year plan (2001–2005) by the Chinese government. It is projected that all rural residents will have access to safe public drinking water by 2020 (World Bank 2006). However, results of the published studies have not been widely disseminated. Four studies published in English (Li XS et al. 1995; Lu et al. 2000; Xiang et al. 2003; Zhao et al. 1996) were cited in a recent report from the NRC (2006), whereas the World Health Organization (2002) has considered only two (Li XS et al. 1995; Zhao et al. 1996) in its most recent monograph on fluoride. Fluoride readily crosses the placenta (Agency for Toxic Substances and Disease Registry 2003). Fluoride exposure to the developing brain, which is much more susceptible to injury caused by toxicants than is the mature brain, may possibly lead to permanent damage (Grandjean and Landrigan 2006). In response to the recommendation of the NRC (2006), the U.S. Department of Health and Human Services (DHHS) and the U.S. EPA recently announced that DHHS is proposing to change the recommended level of fluoride in drinking water to 0.7 mg/L from the currently recommended range of 0.7–1.2 mg/L, and the U.S. EPA is reviewing the maximum amount of fluoride allowed in drinking water, which currently is set at 4.0 mg/L (U.S. EPA 2011). To summarize the available literature, we performed a systematic review and meta-analysis of published studies on increased fluoride exposure in drinking water associated with neurodevelopmental delays. We specifically targeted studies carried out in rural China that have not been widely disseminated, thus complementing the studies that have been included in previous reviews and risk assessment reports. Go to:
METHODS
Search strategy. We searched MEDLINE (National Library of Medicine, Bethesda, MD, USA; http://www.ncbi.nlm.nih.gov/pubmed), Embase (Elsevier B.V., Amsterdam, the Netherlands; http://www.embase.com), Water Resources Abstracts (Proquest, Ann Arbor, MI, USA; http://www.csa.com/factsheets/water-resources-set-c.php), and TOXNET (Toxicology Data Network; National Library of Medicine, Bethesda, MD, USA; http://toxnet.nlm.nih.gov) databases to identify studies of drinking-water fluoride and neurodevelopmental outcomes in children. In addition, we searched the China National Knowledge Infrastructure (CNKI; Beijing, China; http://www.cnki.net) database to identify studies published in Chinese journals only. Key words included combinations of “fluoride” or “drinking water fluoride,” “children,” “neurodevelopment” or “neurologic” or “intelligence” or “IQ.” We also used references cited in the articles identified. We searched records for 1980–2011. Our literature search identified 39 studies, among which 36 (92.3%) were studies with high and reference exposure groups, and 3 (7.7%) studies were based on individual-level measure of exposures. The latter showed that dose-related deficits were found, but the studies were excluded because our meta-analysis focused on studies with the high- and low-exposure groups only. In addition, two studies were published twice, and the duplicates were excluded.Inclusion criteria and data extraction. The criteria for inclusion of studies included studies with high and reference fluoride exposures, end points of IQ scores or other related cognitive function measures, presentation of a mean outcome measure, and associated measure of variance [95% confidence intervals (CIs) or SEs and numbers of participants]. Interpretations of statistical significance are based on an alpha level of 0.05. Information included for each study also included the first author, location of the study, year of publication, and numbers of participants in high-fluoride and low-fluoride areas. We noted and recorded the information on age and sex of children, and parental education and income if available. Statistical analysis. We used STATA (version 11.0; StataCorp, College Station, TX, USA) and available commands (Stern 2009) for the meta-analyses. A standardized weighted mean difference (SMD) was computed using both fixed-effects and random-effects models. The fixed-effects model uses the Mantel–Haenszel method assuming homogeneity among the studies, whereas the random-effects model uses the DerSimonian and Laird method, incorporating both a within-study and an additive between-studies component of variance when there is between-study heterogeneity (Egger et al. 2001). The estimate of the between-study variation is incorporated into both the SE of the estimate of the common effect and the weight of individual studies, which was calculated as the inverse sum of the within and between study variance. We evaluated heterogeneity among studies using the I2 statistic, which represents the percentage of total variation across all studies due to between-study heterogeneity (Higgins and Thompson 2002). We evaluated the potential for publication bias using Begg and Egger tests and visual inspection of a Begg funnel plot (Begg and Mazumdar 1994; Egger et al. 1997). We also conducted independent meta-regressions to estimate the contribution of study characteristics (mean age in years from the age range and year of publication in each study) to heterogeneity among the studies. The scoring standard for the Combined Raven’s Test–The Rural edition in China (CRT-RC) test classifies scores of ≤ 69 and 70–79 as low and marginal intelligence, respectively (Wang D et al. 1989). We also used the random-effects models to estimate risk ratios for the association between fluoride exposure and a low/marginal versus normal Raven’s test score among children in studies that used the CRT-RC test (Wang D et al. 1989). Scores indicating low and marginal intelligence (≤ 69 and 70–79, respectively) were combined as a single outcome due to small numbers of children in each outcome subgroup.
Results
Six of the 34 studies identified were excluded because of missing information on the number of subjects or the mean and variance of the outcome [see Figure 1 for a study selection flow chart and Supplemental Material, Table S1 (http://dx.doi.org/10.1289/ehp.1104912) for additional information on studies that were excluded from the analysis]. Another study (Trivedi et al. 2007) was excluded because SDs reported for the outcome parameter were questionably small (1.13 for the high-fluoride group, and 1.23 for the low-fluoride group) and the SMD (–10.8; 95% CI: –11.9, –9.6) was > 10 times lower than the second smallest SMD (–0.95; 95% CI: –1.16, –0.75) and 150 times lower than the largest SMD (0.07; 95% CI: –0.083, 0.22) reported for the other studies, which had relatively consistent SMD estimates. Inclusion of this study in the meta-analysis resulted with a much smaller pooled random-effects SMD estimate and a much larger I2 (–0.63; 95% CI: –0.83, –0.44, I2 94.1%) compared with the estimates that excluded this study (–0.45; 95% CI: –0.56, –0.34, I2 80%) (see Supplemental Material, Figure S1). Characteristics of the 27 studies included are shown in Table 1 (An et al. 1992; Chen et al. 1991; Fan et al. 2007; Guo et al. 1991; Hong et al. 2001; Li FH et al. 2009; Li XH et al. 2010; Li XS 1995; Li Y et al. 1994; Li Y et al. 2003; Lin et al. 1991; Lu et al. 2000; Poureslami et al. 2011; Ren et al. 1989; Seraj et al. 2006; Sun et al. 1991; Wang G et al. 1996; Wang SH et al. 2001; Wang SX et al. 2007; Wang ZH et al. 2006; Xiang et al. 2003; Xu et al. 1994; Yang et al. 1994; Yao et al. 1996, 1997; Zhang JW et al. 1998; Zhao et al. 1996). Two of the studies included in the analysis were conducted in Iran (Poureslami et al. 2011; Seraj et al. 2006); the other study cohorts were populations from China. Two cohorts were exposed to fluoride from coal burning (Guo et al. 1991; Li XH et al. 2010); otherwise populations were exposed to fluoride through drinking water. The CRT-RC was used to measure the children’s intelligence in 16 studies. Other intelligence measures included the Wechsler Intelligence tests (3 studies; An et al. 1992; Ren et al. 1989; Wang ZH et al. 1996), Binet IQ test (2 studies; Guo et al. 1991; Xu et al. 1994), Raven’s test (2 studies; Poureslami et al. 2011; Seraj et al. 2006), Japan IQ test (2 studies; Sun et al. 1991; Zhang JW et al. 1998), Chinese comparative intelligence test (1 study; Yang et al. 1994), and the mental work capacity index (1 study; Li Y et al. 1994). Because each of the intelligence tests used is designed to measure general intelligence, we used data from all eligible studies to estimate the possible effects of fluoride exposure on general intelligence. Figure 1
Flow diagram of the meta-analysis.
Table 1 Characteristics of epidemiological studies of fluoride exposure and children’s cognitive outcomes.In addition, we conducted a sensitivity analysis restricted to studies that used similar tests to measure the outcome (specifically, the CRT-RC, Wechsler Intelligence test, Binet IQ test, or Raven’s test), and an analysis restricted to studies that used the CRT-RC. We also performed an analysis that excluded studies with co-exposures including iodine and arsenic, or with non-drinking-water fluoride exposure from coal burning. Pooled SMD estimates. Among the 27 studies, all but one study showed random-effect SMD estimates that indicated an inverse association, ranging from –0.95 (95% CI: –1.16, –0.75) to –0.10 (95% CI: –0.25, 0.04) (Figure 2). The study with a positive association reported an SMD estimate of 0.07 (95% CI: –0.8, 0.22). Similar results were found with the fixed-effects SMD estimates. The fixed-effects pooled SMD estimate was –0.40 (95% CI: –0.44, –0.35), with a p-value < 0.001 for the test for homogeneity. The random-effects SMD estimate was –0.45 (95% CI: –0.56, –0.34) with an I2 of 80% and homogeneity test p-value < 0.001 (Figure 2). Because of heterogeneity (excess variability) between study results, we used primarily the random-effects model for subsequent sensitivity analyses, which is generally considered to be the more conservative method [*] (Egger et al. 2001). Among the restricted sets of intelligence tests, the SMD for the model with only CRT-RC tests and drinking-water exposure (and to a lesser extent the model with only CRT-RC tests) was lower than that for all studies combined, although the difference did not appear to be significant. Heterogeneity, however, remained at a similar magnitude when the analyses were restricted (Table 2). Figure 2 Random-effect standardized weighted mean difference (SMD) estimates and 95% CIs of child’s intelligence score associated with high exposure to fluoride. SMs for individual studies are shown as solid diamonds (♦), and the pooled SMD is …Table 2 Sensitivity analyses of pooled random-effects standardized weighted mean difference (SMD) estimates of child’s intelligence score with high exposure of fluoride. Sources of heterogeneity. We performed meta-regression models to assess study characteristics as potential predictors of effect. Information on the child’s sex and parental education were not reported in > 80% of the studies, and only 7% of the studies reported household income. These variables were therefore not included in the models. Among the two covariates, year of publication (0.02; 95% CI: 0.006, 0.03), but not mean age of the study children (–0.02; 95% CI: –0.094, 0.04), was a significant predictor in the model with all 27 studies included. I2 residual 68.7% represented the proportion of residual between-study variation due to heterogeneity. From the adjusted R2, 39.8% of between-study variance was explained by the two covariates. The overall test of the covariates was significant (p = 0.004). When the model was restricted to the 16 studies that used the CRT-RC, the child’s age (but not year of publication) was a significant predictor of the SMD. The R2 of 65.6% of between-study variance was explained by the two covariates, and only 47.3% of the residual variation was attributable to heterogeneity. The overall test of both covariates in the model remained significant (p = 0.0053). On further restriction of the model to exclude the 7 studies with arsenic and iodine as co-exposures and fluoride originating from coal burning (thus including only the 9 with fluoride exposure from drinking water), neither age nor year of publication was a significant predictor, and the overall test of covariates was less important (p = 0.062), in accordance with the similarity of intelligence test outcomes and the source of exposure in the studies included. Although official reports of lead concentrations in the study villages in China were not available, some studies reported high percentage (95–100%) of low lead exposure (less than the standard of 0.01 mg/L) in drinking-water samples in villages from several study provinces (Bi et al. 2010; Peng et al. 2008; Sun 2010). Publication bias. A Begg’s funnel plot with the SE of SMD from each study plotted against its corresponding SMD did not show clear evidence of asymmetry, although two studies with a large SE also reported relatively large effect estimates, which may be consistent with publication bias or heterogeneity (Figure 3). The plot appears symmetrical for studies with larger SE, but with substantial variation in SMD among the more precise studies, consistent with the heterogeneity observed among the studies included in the analysis. Begg (p = 0.22) and Egger (p = 0.11) tests did not indicate significant (p < 0.05) departures from symmetry. Figure 3 Begg’s funnel plot showing individual studies included in the analysis according to random-effect standardized weighted mean difference (SMD) estimates (x-axis) and the SE (se) of each study-specific SMD (y-axis). The solid vertical line indicates …Pooled risk ratios. The relative risk (RR) of a low/marginal score on the CRT-RC test (< 80) among children with high fluoride exposure compared with those with low exposure (16 studies total) was 1.93 (95% CI: 1.46, 2.55; I2 58.5%). When the model was restricted to 9 studies that used the CRT-RC and included only drinking-water fluoride exposure (Chen et al. 1991; Fan et al. 2007; Li XH et al. 2010; Li XS et al. 1995; Li Y et al. 2003; Lu et al. 2000; Wang ZH et al. 2006; Yao et al. 1996, 1997), the estimate was similar (RR = 1.75; 95% CI: 1.16, 2.65; I2 70.6%). Although fluoride exposure showed inverse associations with test scores, the available exposure information did not allow a formal dose–response analysis. However, dose-related differences in test scores occurred at a wide range of water-fluoride concentrations. Go to:
Discussion
Findings from our meta-analyses of 27 studies published over 22 years suggest an inverse association between high fluoride exposure and children’s intelligence. Children who lived in areas with high fluoride exposure had lower IQ scores than those who lived in low-exposure or control areas. Our findings are consistent with an earlier review (Tang et al. 2008), although ours more systematically addressed study selection and exclusion information, and was more comprehensive in a) including 9 additional studies, b) performing meta-regression to estimate the contribution of study characteristics as sources of heterogeneity, and c) estimating pooled risk ratios for the association between fluoride exposure and a low/marginal Raven’s test score. As noted by the NRC committee (NRC 2006), assessments of fluoride safety have relied on incomplete information on potential risks. In regard to developmental neurotoxicity, much information has in fact been published, although mainly as short reports in Chinese that have not been available to most expert committees. We carried out an extensive review that includes epidemiological studies carried out in China. Although most reports were fairly brief and complete information on covariates was not available, the results tended to support the potential for fluoride-mediated developmental neurotoxicity at relatively high levels of exposure in some studies. We did not find conclusive evidence of publication bias, although there was substantial heterogeneity among studies. Drinking water may contain other neurotoxicants, such as arsenic, but exclusion of studies including arsenic and iodine as co-exposures in a sensitivity analysis resulted in a lower estimate, although the difference was not significant. The exposed groups had access to drinking water with fluoride concentrations up to 11.5 mg/L (Wang SX et al. 2007); thus, in many cases concentrations were above the levels recommended (0.7–1.2 mg/L; DHHS) or allowed in public drinking water (4.0 mg/L; U.S. EPA) in the United States (U.S. EPA 2011). A recent cross-sectional study based on individual-level measure of exposures suggested that low levels of water fluoride (range, 0.24–2.84 mg/L) had significant negative associations with children’s intelligence (Ding et al. 2011). This study was not included in our meta-analysis, which focused only on studies with exposed and reference groups, thereby precluding estimation of dose-related effects.The results suggest that fluoride may be a developmental neurotoxicant that affects brain development at exposures much below those that can cause toxicity in adults (Grandjean 1982). For neurotoxicants such as lead and methylmercury, adverse effects are associated with blood concentrations as low as 10 nmol/L. Serum fluoride concentrations associated with high intakes from drinking water may exceed 1 mg/L, or 50 µmol/L—more than 1,000 times the levels of some other neurotoxicants that cause neurodevelopmental damage. Supporting the plausibility of our findings, rats exposed to 1 ppm (50 µmol/L) of water fluoride for 1 year showed morphological alterations in the brain and increased levels of aluminum in brain tissue compared with controls (Varner et al. 1998).
The estimated decrease in average IQ associated with fluoride exposure based on our analysis may seem small and may be within the measurement error of IQ testing. However, as research on other neurotoxicants has shown, a shift to the left of IQ distributions in a population will have substantial impacts, especially among those in the high and low ranges of the IQ distribution (Bellinger 2007).
Our review cannot be used to derive an exposure limit, because the actual exposures of the individual children are not known. Misclassification of children in both high- and low-exposure groups may have occurred if the children were drinking water from other sources (e.g., at school or in the field). The published reports clearly represent independent studies and are not the result of duplicate publication of the same studies (we removed two duplicates). Several studies (Hong et al. 2001; Lin et al. 1991; Wang SH et al. 2001; Wang SX et al. 2007; Xiang et al. 2003; Zhao et al. 1996) report other exposures, such as iodine and arsenic, a neurotoxicant, but our sensitivity analyses showed similar associations between high fluoride exposure and the outcomes even after these studies were excluded. Large tracts of China have superficial fluoride-rich minerals with little, if any, likelihood of contamination by other neurotoxicants that would be associated with fluoride concentrations in drinking water. From the geographic distribution of the studies, it seems unlikely that fluoride-attributed neurotoxicity could be attributable to other water contaminants. Still, each of the articles reviewed had deficiencies, in some cases rather serious ones, that limit the conclusions that can be drawn. However, most deficiencies relate to the reporting of where key information was missing. The fact that some aspects of the study were not reported limits the extent to which the available reports allow a firm conclusion. Some methodological limitations were also noted. Most studies were cross-sectional, but this study design would seem appropriate in a stable population where water supplies and fluoride concentrations have remained unchanged for many years.
The current water fluoride level likely also reflects past developmental exposures. In regard to the outcomes, the inverse association persisted between studies using different intelligence tests, although most studies did not report age adjustment of the cognitive test scores. Fluoride has received much attention in China, where widespread dental fluorosis indicates the prevalence of high exposures. In 2008, the Ministry of Health reported that fluorosis was found in 28 provinces with 92 million residents (China News 2008). Although microbiologically safe, water supplies from small springs or mountain sources created pockets of increased exposures near or within areas of low exposures, thus representing exposure settings close to the ideal, because only the fluoride exposure would differ between nearby neighborhoods. Chinese researchers took advantage of this fact and published their findings, though mainly in Chinese journals and according to the standards of science at the time.
This research dates back to the 1980s, but has not been widely cited
at least in part because of limited access to Chinese journals. [our emphasis]
In its review of fluoride, the NRC (2006) noted that the safety and the risks of fluoride at concentrations of 2–4 mg/L were incompletely documented. Our comprehensive review substantially extends the scope of research available for evaluation and analysis. Although the studies were generally of insufficient quality, the consistency of their findings adds support to existing evidence of fluoride-associated cognitive deficits, and suggests that potential developmental neurotoxicity of fluoride should be a high research priority. Although reports from the World Health Organization and national agencies have generally focused on beneficial effects of fluoride (Centers for Disease Control and Prevention 1999; Petersen and Lennon 2004), the NRC report examined the potential adverse effects of fluoride at 2–4 mg/L in drinking water and not the benefits or potential risks that may occur when fluoride is added to public water supplies at lower concentrations (0.7–1.2 mg/L) (NRC 2006).
In conclusion, our results support the possibility of adverse effects of fluoride exposures on children’s neuro-development. Future research should formally evaluate dose–response relations based on individual-level measures of exposure over time, including more precise prenatal exposure assessment and more extensive standardized measures of neurobehavioral performance, in addition to improving assessment and control of potential confounders.
Go to:
Supplemental Material
(94 KB) PDF
Click here for additional data file.(106K, pdf)
Go to:
Acknowledgments:
We thank V. Malik, Harvard School of Public Health,
for the helpful advice on the meta-analysis methods.
Go to:
Footnotes
This study was supported by internal institutional funds.The authors declare they have no actual or potential competing financial interests.
Go to:
References
-
• Agency for Toxic Substances and Disease Registry. Toxicological Profile for Fluorides, Hydrogen Fluoride, and Fluorine (Update). 2003 Available: http://www.atsdr.cdc.gov/toxprofiles/tp11.pdf[accessed 5 April 2010]
-
• An JA, Mei SZ, Liu AP, Fu Y, Wang CF. Effect of high level of fluoride on children’s intelligence. Chin J Control Endem Dis. 1992;7(2):93–94. [in Chinese]
-
• Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed]
-
• Bellinger DC. Interpretation of small effect sizes in occupational and environmental neurotoxicity: individual versus population risk. Neurotoxicology. 2007;28:245–251. [PubMed]
-
• Bi WJ, Zheng X, Lan TX. Analysis on test results of drinking water’s quality in Janan Railway Bureau from 2005–2009. Prev Med Trib. 2010;16(6):483–485. [in Chinese]
-
• Binet A, Simon T. Shanghai: Commercial Press; 1922. The Measurement of the Mental Development of the Child (translated into Chinese by Jie FP)
-
• Centers for Disease Control and Prevention Achievements in public health, 1990–1999: fluoridation of drinking water to prevent dental caries. MMWR. 1999;48(41):933–940.
-
• Chen YX, Han F, Zhou Z, Zhang H, Jiao X, Zhang S, et al. Research on the intellectual development of children in high fluoride areas. Chin J Control Endem Dis. 1991;6(suppl):99–100. Available: http://www.fluoridealert.org/chinese/ [accessed 20 August 2012]
-
• China News. Twenty-eight provinces were affected by fluorosis in China [in Chinese]. 2008 Available: http://news.qq.com/a/20081216/001707.htm [accessed 3 July 2012]
-
• Chioca LR, Raupp IM, Da Cunha C, Losso EM, Andreatini R. Subchronic fluoride intake induces impairment in habituation and active avoidance tasks in rats. Eur J Pharmacol. 2008;579:196–201. [PubMed]
-
• Ding Y, Gao Y, Sun H, Han H, Wang W, Ji X, et al. The relationships between low levels of urine fluoride on children’s intelligence, dental fluorosis in endemic fluorosis area in Hulunbuir, Inner Mongolia, China. J Hazard Mater. 2011;186:1942–1946. [PubMed]
-
• Egger M, Davey Smith G, Altman DG. London: BMJ Publishing; 2001. Systematic Reviews in Health Care: Meta-Analysis in Context.
-
• Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. [PMC free article] [PubMed]
-
• Fan ZX, Dai HY, Bai AM, Li PO, Li T, LI GD, et al. Effect of high fluoride exposure in children’s intelligence. J Environ Health. 2007;24(10):802–803. [in Chinese]
-
• Grandjean P. Occupational fluorosis through 50 years: clinical and epidemiological experiences. Am J Ind Med. 1982;3(2):227–336. [PubMed]
-
• Grandjean P, Landrigan P. Developmental neurotoxicity of industrial chemicals. Lancet. 2006;368(9553):2167–2178. [PubMed]
-
• Guo XC, Wang R, Cheng C, Wei W, Tang L, Wang Q, et al. A preliminary exploration of IQ of 7–13 year old pupils in a fluorosis area with contamination from burning coal. Chin J Endemiol. 1991;10:98–100. Available: http://www.fluoridealert.org/chinese/ [accessed 20 August 2012]
-
• Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. [PubMed]
-
• Hong F, Cao Y, Yang D, Wang H. A study of fluorine effects on children’s intelligence development under different environments. Chin Prim Health Care. 2001;15:56–57. Available: http://www.fluoridealert.org/chinese/ [accessed 20 August 2012]
-
• Li FH, Chen X, Huang RJ, Xie YP. Intelligence impact of children with endemic fluorosis caused by fluoride from coal burning. J Environ Health. 2009;26(4):338–340. [in Chinese]
-
• Li XH, Hou GQ, Yu B, Yuan CS, Liu Y, Zhang L, et al. Investigation and analysis of children’s intelligence and dental fluorosis in high fluoride area. J Med Pest Control. 2010;26(3):230–231. [in Chinese]
-
• Li XS, Zhi JL, Gao RO. Effect of fluoride exposure on intelligence in children. Fluoride. 1995;28(4):189–192.
-
• Li Y, Jing X, Chen D, Lin L, Wang Z. The effects of endemic fluoride poisoning on the intellectual development of children in Baotou. Chin J Public Health Manag. 2003;19(4):337–338. Available: http://www.fluoridealert.org/chinese/ [accessed 20 August 2012]
-
• Li Y, Li X, Wei S. Effect of excessive fluoride intake on mental work capacity of children and a preliminary study of its mechanism. J West China Univ Med Sci. 1994;25(2):188–191. Available:
Neuro-developmental disabilities, including autism, attention-deficit hyperactivity disorder, dyslexia, and other cognitive impairments, affect millions of children worldwide, and some diagnoses seem to be increasing in frequency. Industrial chemicals that injure the developing brain are among the known causes for this rise in prevalence.
://www.fluoridealert.org/chinese/ [accessed 20 August 2012] [PubMed]
-
• Lin C, Zhang H. Beijing: Beijing Normal University Press; 1986. Wechsler Children Intelligence Scale. Revised Edition in China.
-
• Lin FF, Ai HT, Zhao HX, Lin J, Jhiang JY, Maimaiti, et al. High fluoride and low iodine environment and subclinical cretinism in Xinjiang. Endem Dis Bull. 1991;6(2):62–67. [in Chinese]
-
• Lu Y, Sun ZR, Wu LN, Wang X, Lu W, Liu SS, et al. Effect of high-fluoride water on intelligence in children. Fluoride. 2000;33(2):74–78. [in Chinese]
-
• Mullenix PJ, Denbesten PK, Schunior A, Kernan WJ. Neurotoxicity of sodium fluoride in rats. Neurotoxicol Teratol. 1995;17:169–177. [PubMed]
-
• NRC (National Research Council) Washington, DC: National Academies Press; 2006. Fluoride in Drinking Water: A Scientific Review of EPA’s Standards.
-
• Peng YP, Zou J, Yang DF, Li XH, Wu K. Analysis of water quality from homemade wells in Leshan downtown during 2004–2006. J Occup Health Damage. 2008;23(4):219–221. [in Chinese]
-
• Petersen PE, Lennon MA. Effective use of fluorides for the prevention of dental caries in the 21st century: the WHO approach. Community Dent Oral Epidem. 2004;32(5):319–321. [PubMed]
-
• Poureslami HR, Horri A, Atash R. High fluoride exposure in drinking water: effect on children’s IQ, one new report. Int J Pediatr Dent. 2011;21(suppl 1):47.
-
• Raven J, Raven JC, Court JH. San Antonio, TX:Harcourt Assessment. 2003. Manual for Raven’s Progressive Matrices and Vocabulary Scales.
-
• Ren DL, Li K, Lin D. An investigation of intelligence development of children aged 8–14 years in high-fluoride and low-iodine areas. Chin J Control Endem Dis. 1989;4:251. Available: http://www.fluoridealert.org/chinese/ [accessed 20 August 2012]
-
• Seraj B, Shahrabi M, Falahzade M, Falahzade FP, Akhondi N. Effect of high fluoride concentration in drinking water on children’s intelligence. J Dental Med. 2006;19(2):80–86. [abstract in English]. Available: http://journals.tums.ac.ir/upload_files/pdf/_/2530.pdf [accessed 24 August 2012]
-
• Stern JAC. College Station, TX:Stata Press. 2009. Meta-analysis in Stata: An Updated Collection from the Stata Journal.
-
• Sun LY. Survey of drinking water quality in Jintang County. J Occup Health Damage. 2010;25(5):277–280. [in Chinese]
-
• Sun MM, Li SK, Wang YF, Li FS. Measurement of intelligence by drawing test among the children in the endemic area of Al-F combined toxicosis. J Guiyang Med College. 1991;16(3):204–206. [in Chinese]
-
• Tang QQ, Du J, Ma HH, Jiang SJ, Zhou XJ. Fluoride and children’s intelligence: a meta-analysis. Bio Trace Elem Res. 2008;126:115–120. [PubMed]
-
• Trivedi MH, Verma RJ, Chinoy NJ, Patel RS, Sathawara NG. Effect of high fluoride water on intelligence of school children in India. Fluoride. 2007;40(3):178–183.
-
• U.S. EPA. EPA and HHS Announce New Scientific Assessments and Actions on Fluoride: Agencies Working Together to Maintain Benefits of Preventing Tooth Decay while Preventing Excessive Exposure. 2011 Available: http://yosemite.epa.gov/opa/admpress.nsf/bd4379a92ceceeac8525735900400c27/86964af577c37ab285257811005a8417!OpenDocument [accessed 7 January 2011]
-
• Varner JA, Jensen KF, Horvath W, Isaacson RL. Chronic administration of aluminum-fluoride or sodium-fluoride to rats in drinking water: alterations in neuronal and cerebrovascular integrity. Brain Res. 1998;784:284–298. [PubMed]
-
• Wang D, Di M, Qian M. Tianjin, China: Tianjin Medical University; 1989. Chinese Standardized Raven Test, Rural Version.
-
• Wang G, Yang D, Jia F, Wang H. Research on intelligence quotient of 4-7 year-old children in a district with a high level of fluoride. Endem Dis Bull. 1996;11:60–62. Available: http://www.fluoridealert.org/chinese/ [accessed 20 August 2012]
-
• Wang SH, Wang LF, Hu PY, Guo SW, Law SH. Effects of high iodine and high fluorine on children’s intelligence and thyroid function. Chin J Endemiol. 2001;20(4):288–290. [in Chinese]
-
• Wang SX, Wang ZH, Cheng XT, Li J, Sang ZP, Zhang XD, et al. Arsenic and fluoride exposure in drinking water: children’s IQ and growth in Shanyin County, Shanxi Province, China. Environ Health Perspect. 2007;115:643–647. [PMC free article] [PubMed]
-
• Wang ZH, Wang SX, Zhang XD, Li J, Zheng XT, Hu CM, et al. Investigation of children’s growth and development under long-term fluoride exposure. Chin J Control Endem Dis. 2006;21(4):239–241. [in Chinese; abstract in English]
-
• World Bank. Water Quality Management: Policy and Institutional Considerations. 2006 Available: http://siteresources.worldbank.org/INTEAPREGTOPENVIRONMENT/Resources/China_WPM_final_lo_res.pdf [accessed 13 June 2012]
-
• World Health Organization. Fluorides. Geneva:World Health Organization. 2002 Available: http://whqlibdoc.who.int/ehc/WHO_EHC_227.pdf [accessed 5 September 2012]
-
• Wu TM. Shanghai: Commercial Press (in Chinese); 1936. Second revision of Chinese-Binet Intelligence Test.
-
• Wu T. Beijing: Beijing University Press; 1983. The Chinese Comparative Intelligence Test Guidebook. 3rd ed.
-
• Xiang Q, Liang Y, Chen L, Wang C, Chen B, Chen X, et al. Effect of fluoride in drinking water on children’s intelligence. Fluoride. 2003;36(2):84–94.
-
• Xu YL, Lu CS, Zhang XN. Effect of fluoride on children’s intelligence. Endem Dis Bull. 1994;2:83–84. [in Chinese]
-
• Yang Y, Wang X, Guo X, Hu P. Effects of high iodine and high fluorine on children’s intelligence and the metabolism of iodine and fluorine. Chin J Pathol. 1994;15(5):296–298. Available: http://www.fluoridealert.org/chinese/ [accessed 20 August 2012] [PubMed]
-
• Yao LM, Deng Y, Yang SY, Zhou JL, Wang SL, Cui JW. Comparison of children’s health and intelligence between the fluorosis areas with and without altering water sources. Lit Inf Prev Med. 1997;3(1):42–43. [in Chinese]
-
• Yao LM, Zhou JL, Wang SL, Cui KS, Lin FY. Analysis of TSH levels and intelligence of children residing in high fluorosis areas. Lit Inf Prev Med. 1996;2(1):26–27. [in Chinese]
-
• Zhang J, Gung Y, Guo J. Beijing: Captial Institute of Pediatrics Heatlh Research Office; 1985. Children Intelligence Scale Handbook.
-
• Zhang JW, Yao H, Chen Y. Effect of high level of fluoride and arsenic on children’s intelligence. Chin J Public Health. 1998;17(2):57. [in Chinese]
-
• Zhang M, Wang A, Xia T, He P. Effects of fluoride on DNA damage, S-phase cell-cycle arrest and the expression of NF-κB in primary cultured rat hippocampal neurons. Toxicol Lett. 2008;179:1–5. [PubMed]
-
• Zhao LB, Liang GH, Zhang DN, Wu XR. Effect of a high fluoride water supply on children’s intelligence. Fluoride. 1996;29(4):190–192.
[*] Human variability
Articles from Environmental Health Perspectives are provided here courtesy of
National Institute of Environmental Health Science – Thank you AFS
See also:
— FLUOROSIS —
COAL BURNING – CHINA
106 Fluoride Vol. 36 No. 2 106-112 2003 Research Report
My Views on the Fluoridation of Water
Fluoridation, 1979 Scientific Criticisms and Dangers
by
Philip R.N. Sutton Former Senior Lecturer in Dental Science
University of Melbourne Australia
→ Fluoridation Philip Sutton ←
An Inconvenient Tooth – Fluoride Documentary
↓ ↓
http://www.youtube.com/watch?v=sh-oeu2L8yM&feature=player_embedded
FLUORIDE IN DRINKING WATER:
A Scientific Review of EPA’s Standards
by
Committee on Fluoride in Drinking Water
Board on Environmental Studies and Toxicology
Division on Earth and Life Studies
NATIONAL RESEARCH COUNCIL OF THE NATIONAL ACADEMIES
→ → NRC_2006 ← ←
SEE OUR COMPILATION ON LEAD AND FLUORIDES → HERE
See also → ATRAZINE AND CHLORINE.
Plumb-solvency Exacerbated by Fluoridation-Dr. Geoff Pain
Fluorosis in 89% Carnarvon Aborigines +
Bone/joint problems-Fluorosis
WATER -Stroke & Heart Attacks – a short read
You may not be able to imagine that borax, this humble insecticide
and laundry detergent, has the potential of singlehandedly
bringing down our entire economic system ! ↓
THE BORAX CONSPIRACY
~ DISCLAIMER ~
Some of the articles or pieces posted on this site contain copyrighted material.
Credit is given to the author and links are provided to the original source.
We believe that this constitutes a ‘fair use’.
The peoples of the world have a right to true science.
Deceit and fake $cience need to be exposed.